Drug pricing is an economic issue that has been taken up by AIDS activists. Over the past decade, AIDS activists internationally have been very effective in advocating for reductions in the cost of first-line antiretroviral regimens by pushing for change to global trade agreements, acting as amicus curiae in court cases and involving themselves in vocal popular protests. This popular pressure was most effective when it was combined with competition from generic drug manufacturers and negotiations for voluntary price reductions in branded medicines led by the Clinton Foundation’s H.I.V./AIDS Initiative (CHAI).
However, these gains cannot justify complacency in this area. H.I.V. eventually mutates around antiretroviral drugs, a process that leads to the development of drug-resistant strains of the virus. It is estimated that 10 to 15 percent of people living with the disease require the newer, better-tolerated, second-line drugs after their first four to five years on combination antiretroviral therapy (AVERT 2009).
Second-line drugs such as Kaletra and Efavirenz are frequently ten times more expensive than older first-line regimens (WHO, UNICEF and UNAIDS 2008: 32-5). This is because the patents on second-line drugs remain in force. Patents enforce the exclusive legal right of a company to produce a drug, and thereby inflate drug prices by prohibiting generic production. The World Trade Organization’s Trade Related Aspects of Intellectual Property agreement (TRIP) forces developing countries such as South Africa to move towards greater enforcement of patents. While the agreement allows for the issuing of compulsory licences where there are public health emergencies, many developing countries have been hesitant to take up these flexibilities for fear of actions that would jeopardize their ongoing trade negotiations with wealthier countries, such as being placed on the U.S. Trade Representative’s “watch list,” which happened to Brazil, Thailand and South Africa. Governments in developing countries have good reason to fear threats from Western multinational pharmaceutical companies that they will withdraw from their markets, as actually happened in Thailand (AVERT 2009). One way around this problem is for developing countries to collectively issue compulsory licenses to prevent individual countries from being punished, and to pool their resources for the sustainable production of generic antiretrovirals.
The need to reduce the price of antiretrovirals through such measures is critical to the realization of women’s rights and gender equality in South Africa for two reasons. First, more women than men are living with H.I.V. in South Africa, and in this context a lack of access to affordable second-line antiretrovirals is a critical women’s health issue. Second, it is mostly poor women who bear the social impact of lack of access to second-line antiretrovirals, because they perform most of the unpaid labor of caring for those who are ill with AIDS and the orphaned children many adults leave behind after dying from preventable AIDS-related opportunistic infections.
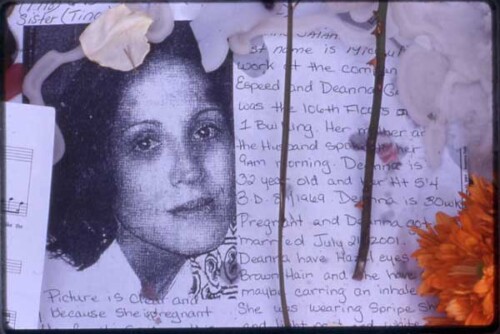
In this regard, it is important to note that just because the home-based care provided by many NGOs is free, through unpaid “volunteers,” it is far from free for the women who undertake such work, as they are mostly poor and unemployed. The time such women spend caring for sick community members and relatives is time not spent developing their skills or seeking paid employment. Such “volunteerism” is not entirely voluntary, as home-based careers are usually driven by a woman’s desire to keep their community and family members, and themselves, alive. In our 2005 ethnographic study, one woman activist described her experience of working as a “voluntary” home-based care worker as follows:
You wake up in the morning, you are hungry. You go to bathe a very sick person . . . you have nothing in your stomach. You have to feed that person. You have to wash them. And you even have to wash their clothes. But you don’t get paid. And the government says it’s because you are doing voluntary work, and that’s not fair (interview, April 26, 2005; Mbali and Connor 2007).
Dr. Olagoke Akintola has pointed out:
The burden of caring for the sick weighs disproportionately on women not only because they are the main providers of care in homes, but also because many have lost their male partners or have never been married, and therefore have to bear alone the financial costs of caring for self and sick family members (2004: 4).
He has gone on to argue that men rarely assist in caring for the sick, both because they are often involved in formal or informal income-generating activities, and because it is not socially expected for them to do so (Akintola 2004: 4).
The problems experienced by home-based caregivers graphically illustrate how poor women bear most of the impact of insufficient social grant provision and the inflated prices of second-line antiretrovirals. While successful advocacy around these issues may take some time, in the interim, NGOs working on AIDS that are concerned about reducing new H.I.V. infections should avoid entrenching women’s economic marginalization by disproportionately relying on their unpaid labor in home-based care programs.