A Salt Lake City police officer arrested registered nurse Alex Wubbels after Wubbels refused to allow him to take a blood sample from a sedated patient without a warrant from a judge or the patient’s consent. 1 “I’m a health care worker,” Wubbels said. “The only job I have is to keep my patients safe.” Her act of courage and patient protection made national news.
Not all hospital workers recognize their ethical obligations to protect patient privacy and to act in their patients’ best interests, however, especially when it comes to pregnant patients. 2 As we describe in this article, some health care providers fail to question – much less oppose – law enforcement requests for private patient information without consent, a warrant, a subpoena, or a court order. All too often, medical staff takes it upon themselves to gather information and share it with police, prosecutors, and others with the power to deprive pregnant people and new parents of their fundamental rights. While a pregnant person might expect that their medical health is a private matter and that a health care provider will respect provider-patient confidentiality, this is often not the case. On many occasions, the arrest of a pregnant woman is precipitated by notification of police or child protective services by a health care provider acting on their own initiative or as part of an effort coordinated with police and prosecutors. In this article, we lay out the circumstances in which these breaches take place, as well as some of their harmful consequences.
Major public health and medical organizations are united in their opposition to the use or threat of policing and punishment as a way to address health concerns about pregnant women. 3 They have been less vocal in opposing the investigations and surveillance that may stem from medical professionals reporting a pregnant patient to the authorities and may lead to family separation. The American College of Obstetrics and Gynecology Committee on Underserved Women, however, unequivocally states that “seeking obstetric-gynecologic care should not expose a woman to criminal or civil penalties,” including incarceration or the loss of custody of her children. 4
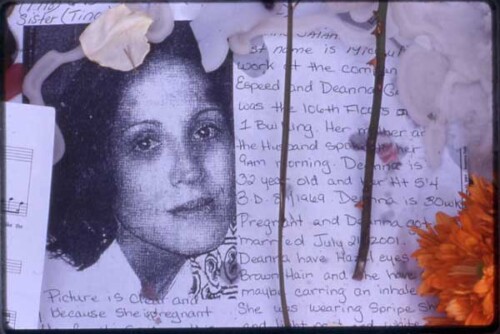
The Universal Declaration of Human Rights states that “all human beings are born free and equal in dignity and rights.” 5 A pregnant person should not, in practice, have a special, lesser status or expectation when it comes to medical care and patient privacy or any other right. Yet National Advocates for Pregnant Women has documented more than a thousand arrests, forced medical interventions, and other deprivations of liberty that would not have occurred but for the fact that the person targeted was pregnant – many of which involved health care workers.
Pregnant low-income women, Black women, and other women of color have been disproportionately targeted for such arrests and are thus disproportionately harmed by their consequences. 6 Women are being denied core constitutional and human rights – including the rights to life, liberty, bodily integrity, and due process of law – based solely on their pregnancy status. These arrests and other punitive state actions are typically justified by reference to anti-abortion and related laws, or ideology that treats the fertilized egg, embryo, or fetus as if it were completely and legally separate from the pregnant woman herself. In other words, in an effort to recriminalize some or all abortions – and the people who have them – pregnancy is used to transform otherwise legal actions (such as attempting suicide, falling down the stairs, consuming alcohol or any criminalized substance), or inactions (such as not getting sufficient bed rest or not consenting to a Cesarean surgery) into crimes against the state.
In nearly half of cases that involved Black women in our earlier study for which information was available (but in only slightly more than one-quarter of those involving white women), we found that pregnant women had been reported to the police by a health care provider such as a doctor, nurse, or hospital social worker. 7 Women who have sought help at hospitals after a miscarriage, stillbirth, or abortion attempt have found themselves subject to bedside interrogations and arrests because a hospital worker (typically without any legal obligation to do so) reported them to authorities.
For example, in Georgia, Kenlissia Jones, a young pregnant woman and mother, was arrested, held without bond, and faced a possible charge of “malice murder” based on the claim that she used misoprostol to terminate her pregnancy. Police arrested Jones at the hospital after a social worker contacted them. In Indiana, Purvi Patel arrived at an emergency room bleeding and seeking help. She told hospital workers that she had miscarried but had not brought the fetal remains with her; she had disposed of them in a trash bin near her workplace. With the help of a physician, police found the remains. A police officer later interrogated Patel at the hospital. Patel was accused of attempting an abortion and was arrested and charged with “neglect of a dependent” and feticide based on the claim that she intentionally terminated her own pregnancy. 8 In Arkansas, Anne Bynum experienced a stillbirth at home. She safeguarded the fetal remains and several hours later brought them to a hospital, asking to see a doctor. She was arrested five days later on charges of “concealing a birth” and “abuse of a corpse.” Police (and possibly hospital staff) initially believed that Bynum had sought to have an abortion. 9 In each of these cases, health care professionals’ actions initiated the arrest of a pregnant patient, in stark contrast to Wubbels, who risked arrest in order to protect her patient’s right to privacy and medical treatment.
These health care workers’ reports have emerged against a particular historical backdrop. In the 1980s, abortion opponents recognized that the racial animus directed at some of society’s most devalued members – poor Black women who used a criminalized and demonized substance and gave birth to mythical crack babies – could be effectively leveraged to rally support for pro-fetus laws and policies. 10 Neoliberal policies that privatized and weakened social programs, combined with the inflammatory rhetoric and punitive policies of the war on drugs, laid the groundwork for criminalizing people whose poverty, race, and mental health problems made them vulnerable targets.
In addition to both individual and structural racism, we surmise that a range of additional factors may explain why some health care workers enable rather than resist the policing of pregnant patients. Health care providers and trainees are among those who may assign an inordinate amount of blame on a pregnant person for pregnancy outcomes based on their actions or inactions. This includes the consumption of any amount of a controlled substance, in spite of the lack of scientific evidence that such substances cause unique, inevitable, or irreversible harm to the fetus and even though rates of drug use by pregnant women are comparatively small and similar across race. 11 Providers may be particularly likely to blame Black women for “not taking care of themselves” even though conditions beyond their control – such as poverty and the weathering chronic stress of pervasive racism – are far more likely to provide an explanation for an adverse pregnancy outcome than specific inactions or actions while pregnant. 12
Some providers’ disclosures stem from a misunderstanding of their obligations under civil child welfare laws to report child abuse and neglect (some of which are rooted in false perceptions that becoming pregnant and using certain drugs is equivalent to civil child abuse or neglect), or from a misunderstanding of what state laws require. 13 In other states, this is how the law is written: around two dozen states and the District of Columbia make prenatal exposure to controlled substances as well as (in some states) alcohol a subject of civil child neglect and abuse laws. 14 Some states require health care workers to report to child welfare authorities based solely on evidence of a positive drug test on a woman or her newborn. In many states, reporting takes place even though the law does not mandate it.
Sometimes the disclosures stem from an explicit collaboration between hospital staff and law enforcement. For instance, until the practice was deemed unconstitutional, South Carolina hospital workers searched pregnant women for evidence of drug use without a warrant or consent under the guise of medical testing, turned that information over to the police along with other highly personal medical information, and then helped police arrest pregnant women and new mothers. The policy resulted in the arrests of at least thirty patients, all but one of whom were Black. In 2001, the US Supreme Court, in Ferguson v. City of Charleston, decided that these practices violated a patient’s Fourth Amendment rights to be free from unreasonable search and seizure. 15
More recently, in Alabama, pregnant women seeking care in hospitals in certain counties, as well as new mothers and their newborns, have been drug tested and subjected to searches without their consent. Hundreds of women have been arrested under a radical judicial expansion of the state’s Chemical Endangerment of a Child law. 16 The 2006 law was passed to punish adults who brought children to dangerous places such as meth labs. The Alabama Supreme Court, however, ruled that the word “child” includes the unborn from the moment of fertilization, empowering law enforcement officials to use the law to arrest anyone who becomes pregnant and uses any amount of a controlled substance. 17 As a result, a woman who used half a Valium, women who were receiving physician-prescribed methadone treatment, a woman who used controlled substances in a suicide attempt that she survived, and a woman who used marijuana as a safer alternative to epilepsy medications that have known risks to fetuses have been arrested and charged. 18 To date, more than 600 pregnant women and new mothers have been arrested, prosecuted, and separated from their children and families under the Alabama law. Almost all of these state responses followed reports from hospital personnel who had no authority to search their pregnant patients; who were under no legal obligation to drug test pregnant people, new parents, or newborns in the first place; and who had no legal obligation to report suspected drug use or drug test results to criminal law authorities.
In 1998, Wisconsin put into effect the Unborn Child Protection Law (Act 292), a law that purports to address problems associated with pregnancy and use of alcohol or a controlled substance. Although it does not require health care providers to test or report women upon finding evidence of pregnancy and of present or past alcohol or drug use, women who have voluntarily sought help at hospitals have been reported to government authorities. As a result, they have been taken into custody for a court hearing where they are not entitled to a lawyer but where their fertilized egg, embryo, or fetus is represented by legal counsel, and have subsequently been locked up, detained, or subjected to forced treatment in county jails and mental hospitals. 19
Medical staff mobilization of law enforcement is an ethical affront to the medical principle of nonmalfeasance (or “do no harm”). The consequences can be fatal. In January 2013, Jamie Lynn Russell, 33, went to the hospital in agonizing pain that prevented her from lying down. Hospital staff perceived her as “noncompliant” and asked a police officer to assist. 20 When police allegedly found that Russell had prescription pain pills that did not belong to her, police took her to jail on charges of drug possession. Within two hours of being behind bars, Russell died of a ruptured ectopic pregnancy.
More commonly, highly sensitive medical information winds up not only in the hands of prosecutors and courts, but in full public view, whether via a single story in the local press or extensive and ongoing local and national coverage. News stories may report drug use, sexually transmitted infection status, and other potentially stigmatizing information. Women whose private medical information is publicly disclosed in this way report stress, humiliation, and the loss of their jobs and reputations. A pregnant woman prosecuted under the Alabama chemical endangerment statute – whose case was later dismissed – observed, “I feel like everywhere I go, people … look at me and shame me like I’m a monster.” 21
Hospital workers’ disclosures lead to further violations of pregnant patients’ rights to physical liberty, bodily autonomy and integrity, informed consent and medical decision-making, due process, and protection from cruel and unusual punishment. 22 They also contribute to an expanding and racist carceral state. The price of these breaches is borne by the same people who are most susceptible to over-policing and ensnarement in a criminal legal system that is extremely punitive and overwhelmingly unable to mete out justice. Pregnant women and new mothers face sanctions and other consequences inflicted by criminal legal and child welfare systems that are harsh and dysfunctional and that target low-income people and people of color. 23 Involuntary family separation causes significant trauma to children and their parents, whether it occurs as a consequence of child welfare involvement or of a parent’s detention or incarceration. 24
The more physicians and nurses become entangled in law enforcement, “the more they resemble agents of the police (and police informants and probation officers) rather than health care professionals.” 25 Such entanglement erodes public trust in the “helping professions” of medicine and social work. This trust is already fragile among many Black, Indigenous, Latinx, immigrant, and low-income communities given experiences of forced sterilization, gynecological and other medical experimentation, and other occasions of medical racism. 26 The collaboration of health care providers with law enforcement officials fuels a climate of mutual suspicion and deters patients from communicating openly with people who might help them secure needed medical services. It also contributes to the toxic weathering stress of structural racism that is increasingly recognized as playing a major role in the obscenely high rates of infant mortality, maternal death, and serious pregnancy complications among Black women in the United States. 27
Pregnant women and new parents deserve better than this. They need support, not surveillance. The situation challenges each of us to mobilize to secure universal and patient-centered health care for all people, and to defend pregnant people and families against violations of their civil and human rights. 28
Health care providers, in particular, bear responsibility for pregnant patients’ health and wellbeing and for respecting their rights and dignity. The American Nurses Association Code of Ethics stipulates that a nurse’s “primary commitment is to the patient” and requires that a nurse “promotes, advocates and protects the rights, health and safety” of the patient. 29 Physicians are expected to challenge unjust laws and policies. The American College of Obstetrics and Gynecology Committee on Underserved Women urges physicians to work with policymakers and legislators to retract punitive mandatory reporting policies and laws. The American Medical Association recognizes that “in some cases, the law mandates conduct that is ethically unacceptable. According to the American Medical Association, “When physicians believe a law violates ethical values or is unjust, they should work to change the law.” Its code of ethics continues: “In exceptional circumstances of unjust laws, ethical responsibilities should supersede legal duties.” 30
People who seek medical attention for any aspect of pregnancy – including prenatal care, labor and birth, miscarriage, stillbirth, or abortion – should not have to fear arrest. As Jean Ross, copresident of National Nurses United, points out: “The first job of a registered nurse is always to protect and advocate for her patient, period.” 31 If ordered or pressured by a law enforcement official, a colleague, or anyone else to violate their pregnant patients’ rights, health workers should follow the example set by Wubbels and the hospital at which she worked: Speak up and defend the patient. 32
- Derek Hawkins, “‘This Is Crazy,’ Sobs Utah Hospital Nurse as Cop Roughs Her up, Arrests Her for Doing Her Job,” Washington Post, 2 September 2017. The police officer sought to determine the patient’s blood alcohol level.[↑]
- National Advocates for Pregnant Women recognizes that not all people with the capacity for pregnancy identify as women. We fight to win human rights of all people and to ensure that pregnancy is not a basis for denying any person their civil and human rights. Because the people NAPW has thus far represented identify as cisgender women, we specifically refer to pregnant women in this article. This in no way is intended to erase or deny the experiences of pregnant people who do not identify as women, and we believe all pregnant people are entitled to the same protections we advance here. We will continue to explore the best ways to use language and our voice to challenge the harmful effects of an inflexible gender binary. We are grateful to the two anonymous reviewers, issue editors Andrea J. Ritchie and Levi Craske, and Amber Khan and Nancy Rosenbloom of National Advocates for Pregnant Women for their helpful comments on earlier drafts.[↑]
- National Advocates for Pregnant Women, “Medical and Public Health Group Statements Opposing Prosecution and Punishment of Pregnant Women,” March 2017, http://advocatesforpregnantwomen.org/Medical%20and%20Public%20Health%20Group%20Statements%20revised%20March%202017.pdf.[↑]
- American College of Gynecologists and Obstetricians, “Substance Use Reporting and Pregnancy: The Role of the Obstetrician-Gynecologist. Committee Opinion 473,” Obstetrics and Gynecology 117 (2011, reaffirmed 2014): 200.[↑]
- United Nations, Universal Declaration of Human Rights, https://www.un.org/en/udhrbook.[↑]
- Lynn M. Paltrow and Jeanne Flavin, “Arrests of and Forced Interventions on Pregnant Women in the United States, 1973–2005: Implications for Women’s Legal Status and Public Health,” Journal of Health Politics, Policy, and Law 38, 2 (2013): 299.[↑]
- White women were far more likely to have their cases come to the attention of the police through reports by a probation or parole officer, an arrest unrelated to pregnancy, or a report from a boyfriend or family member. Paltrow and Flavin, “Arrests of and Forced Interventions on Pregnant Women,” 311, 313. The hypervigilance regarding Black women’s behavior has been documented on other occasions and in other settings. See “From ‘BBQ Becky’ to ‘Golfcart Gail,’ List of Unnecessary 911 Calls Made on Blacks Continues to Grow,” ABC News, 19 October 2018, https://abcnews.go.com/US/bbq-becky-golfcart-gail-list-unnecessary-911-calls/story?id=58584961.[↑]
- Emily Bazelon, “Purvi Patel Could Be Just the Beginning,” New York Times Magazine, 1 April 2015. Patel was accused of attempting to have an abortion and was convicted of two crimes: feticide and neglect of a dependent. The feticide conviction was later overturned.[↑]
- New York Times Editorial Board, “How My Stillbirth Became a Crime,” New York Times, 28 December 2018.[↑]
- Lynn M. Paltrow, “Pregnant Drug Users, Fetal Persons, and the Threat to Roe v. Wade,” Albany Law Review 62 (1999): 999–1055.[↑]
- Lynn Paltrow and Kathrine Jack, “Pregnant Women, Junk Science, and Zealous Defense,” Champion, May 2000, 1–10; SAMHSA, Results from the 2017 National Survey on Drug Use and Health: Detailed Tables (Washington, DC: SAMHSA, 2018), https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf.[↑]
- Carolyn Sufrin, Jailcare: Finding the Safety Net for Women behind Bars (Oakland, CA: University of California Press, 2017). Furthermore, pregnancy loss is a common, even natural experience. As many as half of all conceptions end in miscarriage, the cause of which is most often a deadly chromosomal abnormality unrelated to the parents. Pre-existing medical conditions (such as diabetes) play a role in the health of pregnant women and pregnancy outcomes, as do pre-existing social conditions. Barbara Katz Rothman, Bun in the Oven: How the Food and Birth Movements Resist Industrialization (New York: NYU Press, 2016); Jeanne Flavin and Lynn M. Paltrow, “Punishing Pregnant Drug-Using Women: Defying Law, Medicine, and Common Sense,” Journal of Addictive Diseases 29, 2 (2010): 231–44.[↑]
- Child Welfare Information Gateway, Mandatory Reporters of Child Abuse and Neglect (Washington, DC: US Department of Health and Human Services, Children’s Bureau, n.d.), https://www.childwelfare.gov/pubpdfs/manda.pdf. Child Abuse Prevention and Treatment Act (CAPTA), federal legislation that addresses child abuse and neglect, requires states to have a policy in place to report some substance-exposed newborns in exchange for receiving federal funding. Nothing in CAPTA, however, requires reporting of all substance-exposed newborns as suspected abuse or neglect. CAPTA reporting is for the purpose of providing services where needed, and the law explicitly says it does not create a definition under federal law of abuse or neglect. One requirement is that states confirm in writing that they have implemented certain policies and procedures “including appropriate referrals to child protection service systems” of “infants born with and identified as being affected by substance abuse or withdrawal symptoms resulting from prenatal drug exposure, or a Fetal Alcohol Spectrum Disorder” (emphasis added). Nothing in the federal law, however, requires reporting based only on a positive toxicology (of either mother or infant) or a known history of substance use. Nothing in CAPTA requires that drug use and medications to treat dependency problems by pregnant women in and of themselves be reported as child abuse or neglect. Moreover, nothing in CAPTA prohibits states from creating a reporting mechanism that is not and, more importantly, may not by itself be the basis of an abuse or neglect finding. Unfortunately, we know of no state where reports to child protective services may not lead to investigation or suspicion of abuse or neglect. Indeed, there are many states in which, under state law, drug use and drug treatment (methadone, buprenorphine) during pregnancy must be reported to child protective services as suspected child abuse or neglect. Email correspondence between Nancy Rosenbloom of National Advocates for Pregnant Women and the authors, 18 May 2018.[↑]
- See Guttmacher Institute, Substance Use during Pregnancy, 1 April 2019, https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy. See also Child Welfare Information Gateway, Parental Drug Use as Child Abuse (Washington, DC: US Department of Health and Human Services, Children’s Bureau, 2016), https://www.childwelfare.gov/topics/systemwide/laws-policies/statutes/drugexposed/.[↑]
- Ferguson v. City of Charleston, 2001, 532 US 67, Oyez, https://www.oyez.org/cases/2000/99-936.[↑]
- Nina Martin, “Alabama Mom’s Charges Dropped but Only after Arduous Battle,” ProPublica, 2 June 2016, https://www.propublica.org/article/alabama-moms-charges-are-dropped-but-only-after-an-arduous-battle; Nina Martin, “How Some Hospitals Quietly Test New Mothers – Without Their Consent,” ProPublica, 30 September 2015, https://www.propublica.org/article/how-some-alabama-hospitals-drug-test-new-mothers-without-their-consent; Nina Martin, “This Alabama Judge Has Figured out How to Dismantle Roe v. Wade,” ProPublica, 10 October 2014, https://www.propublica.org/article/this-alabama-judge-has-figured-out-how-to-dismantle-roe-v-wade. Amnesty International, Criminalizing Pregnancy: Policing Pregnant Women Who Use Drugs in the United States (New York: Amnesty International, 2017).[↑]
- National Advocates for Pregnant Women, “Press Statement: Lynn Paltrow on Alabama Supreme Court’s Decision in ‘Personhood’ Measure in Disguise Case,” 12 January 2013, http://advocatesforpregnantwomen.org/blog/2013/01/press_release_national_advocat.php.[↑]
- For a firsthand account of this, see Dinah Ortiz in this issue.[↑]
- “The Case of Alicia Beltran,” video, https://vimeo.com/202241357.[↑]
- Adam Kemp, “Family of Pauls Valley Woman Who Died in Police Custody Seeks Answers,” NewsOK, 4 February 2013, http://newsok.com/article/3751456.[↑]
- Nina Martin, “Take a Valium, Lose Your Kid, Go to Jail,” Digg, 23 September 2015, http://digg.com/2015/alabama-drug-laws-pregnant-women.[↑]
- Lynn M. Paltrow, “Roe v. Wade and the New Jane Crow: Reproductive Rights in the Age of Mass Incarceration,” American Journal of Public Health 103, 1 (2013): 17–21. doi: 10.2105/AJPH.2012.301104.[↑]
- See also Dorothy Roberts, Killing the Black Body (New York: Random House, 1997); Dorothy Roberts, Shattered Bonds: The Color of Child Welfare (New York: Basic Books, 2002).[↑]
- Kristen Turney and Christopher Wildeman, “Maternal Incarceration and the Transformation of Urban Family Life,” Social Forces 96, 3 (2018): 1155–82.[↑]
- George J. Annas, American Bioethics: Crossing Human Rights and Health Law Boundaries (Oxford, UK: Oxford University Press, 2005).[↑]
- Deirdre Cooper-Owens, Medical Bondage: Race, Gender, and the Origins of American Gynecology (Athens, GA: University of Georgia Press, 2018); Harriet Washington, Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present (New York: Doubleday, 2006); Kiana Mickles, “Beyond J. Marion Sims: Black Women Have Been Fighting Discrimination in the Medical Industrial Complex for Centuries,” CRWN, October 2017, https://crwnmag.com/blog/2017/10/healing-from-racial-trauma-in-the-fight-for-universal-healthcare; “Medical Racism,” Encyclopedia of Race and Racism, http://www.encyclopedia.com/social-sciences/encyclopedias-almanacs-transcripts-and-maps/medical-racism.[↑]
- Linda Villarosa, “Why America’s Black Mothers and Babies Are in a Life-or-Death Crisis,” New York Times Magazine, 11 April 2018, https://www.nytimes.com/2018/04/11/magazine/black-mothers-babies-death-maternal-mortality.html.[↑]
- Elizabeth Dawes Gay, “On ‘Commonsense Childbirth’: A Q&A with Midwife Jennie Joseph,” Rewire News, 26 July 2016, https://rewire.news/article/2016/07/26/commonsense-childbirth-qa-midwife-jennie-joseph/. For more information, see National Advocates for Pregnant Women, http://www.advocatesforpregnantwomen.org.[↑]
- American Nurses Association, “Code of Ethics,” https://www.nursingworld.org/coe-view-only.[↑]
- American Medical Association, “Preamble,” Code of Medical Ethics Opinions, 2016, https://www.ama-assn.org/sites/default/files/media-browser/preface-and-preamble-to-opinions.pdf.[↑]
- National Nurses United, “Nurses Condemn Police Assault on Utah Hospital RN for Advocating for an Unconscious Patient,” 1 September 2017, press release, https://www.nationalnursesunited.org/press/nurses-condemn-police-assault-utah-hospital-rn-advocating-unconscious-patient.[↑]
- Bill Chappell, “Calling Nurse ‘A Hero,’ Utah Hospital Bars Police from Patient-Care Areas,” National Public Radio, 5 September 2017, https://www.npr.org/sections/thetwo-way/2017/09/05/548601099/calling-nurse-a-hero-utah-hospital-bars-police-from-patient-care-areas.[↑]